9 Best Hacks to a Sound Sleep with Eczema

Skin is the largest organ in the body; it also acts as an armor that offers protection from a plethora of viruses, bacteria, and above all regulates the body temperature. That said, there is a long list of skin conditions that affect humans, out of which eczema tops the list.
Sleeping issues are common in the people suffering from eczema; this further leads to impaired quality of life. Sleep disorder is often considered as one of the key symptoms of eczema.
Let us get acquainted, in detail, with what is eczema, types of eczema, its impact on sleep, key tips to sleep better with this condition, and how to prevent eczema outbreaks.
What is Eczema
The word Eczema is derived from the Greek word which means ‘to boil over,’ and the etymology is dead-on. Eczema cannot be termed as a specific condi tion; rather it is a cumulative term for a group of similar skin disorders that leads to inflammation, scaling, redness, and dryness.
It is not contagious; however, it is advisable to get a correct and timely diagnosis of eczema from a skin specialist. As far as the symptoms are concerned, they are mainly related to the inflammation that occurs on the top layer of the dermis.
Different types of eczema
Eczema is quite common; over 30 million Americans have some form of eczema. Eczema is, at times, called Atopic Dermatitis. There are six types of eczema, and each type has unique symptoms, causes, and treatment.
Let us discuss types of eczema, their symptoms, causes, and treatment.
Venous Eczema (Stasis Dermatitis)

This type is commonly found in older adults, and it mainly affects lower legs. This type of condition is caused by fluid build-up. This swelling leads to redness, pain, itching, and swelling.
Symptoms –
Ø Swelling in the lower part of the legs.
Ø Legs may feel heavy or ache.
Ø Hair loss on shins and ankles.
Ø Irritated skin.
Ø Swollen, itchy, and red skin particularly over varicose veins.
Ø Infection.
Ø Open sores on lower legs and tops of the feet.
Causes –
Ø Blood flow issues in lower legs.
Ø Swollen or enlarged veins.
Ø Congestive Heart Failure (CHF).
Ø Injury to the lower leg.
Ø A blood clot in the lower leg (Deep Vein Thrombosis).
Ø Hypertension.
Ø Kidney Failure.
Ø Obesity.
Treatment –
Ø Wear compression socks to relieve swelling and encourage circulation.
Ø Keeping legs elevated while sleeping.
Ø Using antihistamines to alleviate itching.
Ø Using emollients to moisturize and protect the skin.
Ø For the treatment of infected ulcers, use antibiotics and special dressing.
Nummular Eczema (Discoid Eczema)

In Latin, Nummular means ‘coin’. An individual suffering from Nummular Eczema tends to have round ‘coin shaped’ rashes or sores on the skin. The appearance of this type of eczema is unlike other types, and it is also the itchiest.
These patches are usually seen on the legs, and it is more common during winters. Experts are of the view that this type of eczema occurs more in men than female.
Symptoms –
Ø Chills.
Ø Having a yellow crust over patches.
Ø Skin turning brown, pink or red around the lesions.
Ø Burning and itching, especially at night.
Ø Feeling sick.
Causes –
Ø An individual suffering from Nummular Eczema may suffer from atopic eczema.
Ø Poor blood flow may also worsen the symptoms of Nummular Eczema.
Ø Dry skin.
Ø Increased level of stress.
Ø Surgery.
Ø Various environmental irritants like soaps, formaldehyde, and metals.
Ø Change in temperature.
Treatment –
At the moment, there is no cure for Nummular Eczema. However, making some changes to your lifestyle does help in managing the condition. To control Nummular Eczema, make sure you avoid –
Ø Using fabric softener and dry sheets.
Ø Wool and other irritants.
Ø Stressful situations.
Ø Using harsh soaps.
Ø Exposure to environmental irritants like – chemicals and cleaners.
Ø Using hot water and undue bathing.
Dyshidrotic Eczema
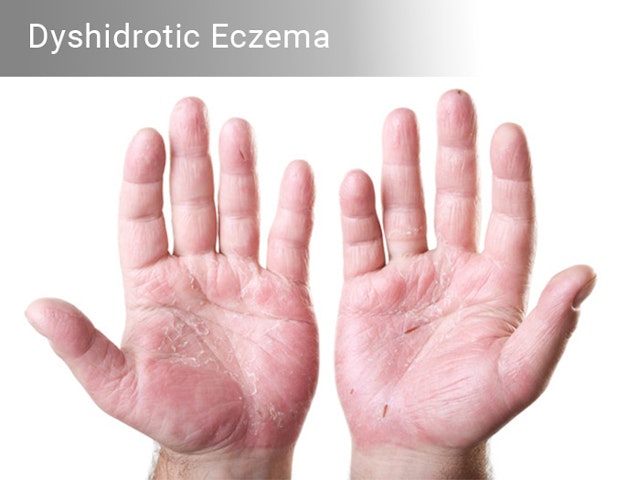
This type of eczema, usually, crops up during winter season. Females are more prone to this type of eczema than men. As per this skin condition, small blisters develop on the palms of hand and soles of the feet. Usually, the blisters are filled with fluid. These blisters may last up to three weeks before drying and can sometimes be large and uncomfortable.
Symptoms –
Itching.
Flaking.
Redness.
Formation of blisters on the edges of palms, fingers, toes.
Pain.
Scaly and cracked skin.
Causes
Ø Pollen.
Ø Increased level of stress.
Ø Seasonal allergies.
Ø Presence of nickel in foods like – soybeans, chocolate, almonds, nuts, etc.
Ø Undue sweating of hands or feet.
Ø Prolonged contact with water.
Treatment –
Ø Using over-the-counter corticosteroids creams. Such creams reduce irritation and skin inflammation.
Ø To reduce itching, you can take antihistamines – Benadryl or Alavert.
Ø Draining blisters is also a treatment, but this ought to be performed by a certified physician as it increases the risk of infections.
Ø Taking oral steroids like – prednisone. It helps in reducing the inflammation.
Contact Dermatitis

Contact Dermatitis usually takes place when the skin gets in touch with an irritant substance or allergen. The skin becomes inflamed, causing it to burn and itch, and eventually turn red. This type of dermatitis is further divided into types – Allergic and Irritant.
When your skin repeatedly gets in touch with a substance that irritates the skin, then it can result in Irritant Contact Dermatitis. And when your immune system reacts to an allergen, then it is the case of Allergic Contact Dermatitis.
Symptoms –
Ø Skin becomes dry, cracked, blistered, and cracked.
Ø Severe itching.
Ø A red rash.
Ø Skin redness.
Ø Sun sensitivity.
Ø Oozing blisters.
Ø Hives.
Contact Dermatitis Causes –
Ø Latex.
Ø Jewelry.
Ø Paint.
Ø Detergents.
Ø Tobacco smoke.
Ø Nickel.
Ø Poison Ivy.
Ø Solvents.
Ø Makeup.
Ø Soaps and perfumes.
Ø Bleach.
Contact Dermatitis Treatment
Your physician will identify the actual cause – whether it’s an allergy to a chemical present in the makeup or it is some metal. Since the exposed areas are the ones affected, your physician will consider the location to make out the actual cause, and he will decide whether you should be given an oral or topical steroid accordingly.
Seborrheic Dermatitis (Seborrheic Eczema and Seborrheic Psoriasis)

An individual with Seborrheic Dermatitis, a chronic form of eczema, usually suffers from an itchy and flaky rash. It also affects the oily areas of your body such as genitals, eyelids, armpits, nose, chest, and ears. This type of skin disease has an appearance similar to psoriasis. This form of skin condition can appear on your body as well as scalp.
Symptoms –
Ø The appearance of dandruff on your scalp, hair, and beard.
Ø Itching.
Ø Inflamed skin.
Ø Greasy skin patches on different body parts such as – eyelids, scalp, face, chest, armpits, and groin.
Ø Pink-colored patches.
Causes –
Exact causes of Seborrheic Dermatitis are still under research. This particular condition may be due to a combination of below-mentioned things –
Ø Certain medical conditions and medicines.
Ø Stress.
Ø Dry, cold weather.
Ø Hormonal changes.
Ø Soaps, chemicals, and harsh detergents.
Ø Irregular response of the immune system.
Treatment –
Physicians have seen seborrheic dermatitis clearing up itself. In some cases, it may last for years. However, the skin condition can be controlled by following a good skin care regimen. Besides, the type of treatment your dermatologist prescribes will vary as per your age and body part where seborrheic dermatitis has appeared.
You can use over-the-counter dandruff shampoos containing the following ingredients –
Ø Ketoconazole.
Ø Zinc pyrithione.
Ø Selenium sulfide.
Ø Coal tar.
Ø Salicylic acid.
Atopic Dermatitis or Atopic eczema

An individual suffering from Atopic Dermatitis tends to have red and itchy skin. It is usually found in children; however, it can occur at any age. What makes this skin condition worse is the fact that it is long lasting and it flares periodically. That said, the skin condition isn’t contagious.
Symptoms –
Ø Itching.
Ø Scaly cracked and thickened skin.
Ø Dry skin.
Ø Cracks behind the ears.
Ø Redness.
Causes –
Ø Hair and saliva of animals.
Ø Food allergies.
Ø Dust mites.
Ø Skin infections, such as scabies.
Ø Dry skin.
Ø Certain fabrics such as – synthetics or woolen.
Ø Extreme changes in temperature.
Ø Tobacco smoke.
Ø Sweating.
Treatment –
Depending on the severity of the condition, your dermatologist may prescribe your injectable, oral, or topical prescription. You may also be suggested following treatments –
Medications – A corticosteroid cream or ointment. In severe conditions, your dermatologist may prescribe prednisone (oral corticosteroids).
Therapies – Your dermatologist may also use different therapies such as – Wet-wrap therapy and Phototherapy.
Prevention of Eczema Flare-Ups
Still, doctors are unable to find a cure for eczema, but with the help of various treatments, symptoms can be reduced considerably and the flare-ups can also be prevented.
Here are some of the important steps you can follow to prevent eczema flare-ups –
Moisturize Your Skin
You can prevent the outbreaks by ensuring your skin is aptly moisturized. Ideally, you should apply a moisturizer after taking a bath and whenever you feel the need. Keeping the moisturizer in the refrigerator will help you enjoy a deeper feeling of relief. Moisturizers tend to feel wonderful when applied cold.
Reduce Elements that Trigger Outbreaks
There are certain factors owing to which outbreaks can be triggered such as – molds, pet dander, dust, mites, certain foods, etc. It is important that you first figure out the factors that trigger the outbreaks and secondly you need to avoid them as much as possible. This will undoubtedly prove beneficial in delaying your next outbreak.
Avoid Scratching
Remember when you scratch, you are only making your itch and eczema worse. Some people scratch so much that they end up bleeding, eventually leading to infection. You can adopt the following methods for itch relief and soothe your skin –
Ø You can make a quick compress that will help cool off your skin. If you want intense relief, you can use an ice pack or take one or two ice cubes in a soft towel and apply on the affected areas. This will help numb the area and controls the irritation.
Ø Using thin lotions will be of no use. Go for an eczema cream or ointment. You can either ask your doctor about the cream you should go for or you can look for words like ‘skin repair’ or ‘barrier cream’ on the labels when you are shopping for a cream.
Ø The sunflower seed oil has shown positive results to soften the skin than any cream. You can also use coconut oil; it helps in nourishment and reduces the inflammation.
Ø If you choose to apply Hydrocortisone, it does alleviate the itching. Make sure you don’t overdo it as it has side effects. Besides, ensure that you have read the directions, on the label, carefully or consulted your physician before using it.
Go for Clothing Made of 100% Cotton
Since cotton lets the skin breath, you should wear clothes made up of 100% cotton. It also comes handy in preventing skin irritation. Ideally, you should wash your new clothes and avoid wool as such material end up irritating the skin.
Be Choosy About Your Facial and Body Products
Not many people are aware of the fact that hair products, shaving creams, perfumes, scented lotions tend to have harmful ingredients that can lead to skin irritation and trigger eczema outbreaks.
The best way to find out whether the product is suitable for your skin, it is advisable to test them on a small area of your skin. Ideally, you should leave the product on your skin for, at least, 24 hours, then check if you have had a reaction.
Manage Your Stress
Stress also induce eczema outbreaks. You can use any method that helps reduce your stress levels. For instance – exercising is one of the easiest ways to unwind.
How Stress may Trigger Eczema?
When considering the relation between stress and eczema, it has been suggested that stress results in a spike in the hormone cortisol. When cortisol (stress hormone) is produced in an excessive amount because of stress, the skin tends to become abnormally oily. As a result, you may encounter an eczema outbreak.
Eczema and Sleep Disruption
Sleep is beneficial for our health, and a healthy adult needs 7 to 9 hours of sleep per night. But, when you are suffering from eczema, you usually face problem having a sound sleep. As per physicians, when you don’t have enough sleep, not only your health and mental well-being suffer, but it worsens your eczema as well.
A survey of around 34,000 adults showed that the people suffering from eczema tend to have more odds of fatigue and insomnia. The study also found that there is an increased risk of workplace accidents and psychological disorders. The outbreak of eczema at night leads to discomfort, eventually making it difficult to sleep.
Reasons for Eczema Flare-up at Night
Researchers are still not confirmed about the exact causes of eczema; however, they support the involvement of both environmental and genetic reasons.
Here are some of the reasons as to why eczema symptoms may feel worse at night –
· People scratch more often in their sleep; this can only worsen the itchiness.
· Your sleep/wake cycle is responsible for decreasing your body temperature at night, therefore making the skin feel itchier.
· If you have used a moisturizer in the day, probably the effects may have worn off by the night time.
· Numerous health-related reasons are also responsible for itchy skin at night. These include –
Ø Lymphoma and Leukemia.
Ø Bed Bugs, Scabies, Pinworms, Lice, etc.
Ø Thyroid Issues.
Ø Pregnancy.
Ø Hives, Psoriasis, Atopic Dermatitis, etc.
Ø Depression, Schizophrenia, and Stress.
Ø Liver or Kidney Disease.
Ø Diabetes, Shingles, and Multiple Sclerosis.
Beneficial Tips for Sleeping Better with Eczema
For any eczema sufferer, nighttime itching and not being able to sleep are some of the most bothersome symptoms. And not surprisingly, lack of sleep can lead to both physical and cognitive issues.
But wait, you don’t have to go through all this. Here are some helpful tips to get some coveted sleep.
Cut Down Nighttime Scratching
Overlooking the little sharp bit of your fingernails is probably the biggest mistake you can make when you are suffering from eczema. It is a good idea to keep your nails short and trim. Besides, it also reduces the damage your skin receives and help you sleep better.
Find the Right Temperature
There is a close relation between eczema and body temperature. When you are too hot, you tend to scratch more. The moment your body temperature gets hotter, it tends to worsen eczema. If you wake up in the middle of the night quite often, then it is because you become overheated. This certainly makes the eczema-related itching worse.
Here are some conducive methods to keep you cool at night –
Ø It is advisable to adjust your thermostat before you sleep. You can choose to turn down the temperature of the AC.
Ø You can opt for automated temperature system. It will help you to decrease the temperature at a specific time every night. Sleep.org did a study and it was found that the ideal temperature for having a sound sleep is 60 and 67 degrees.
As such, there is no universal temperature that is suitable for everyone. You can try setting different temperatures to find the one that suits you while you are asleep.
Apply Moisturizers Before Sleeping
If you don’t moisturize before going to bed, you will probably wake up several times in the night. Ideally, you should apply a thick moisturizer thirty minutes to an hour before going to bed. This will help the moisturizer to go deep into your skin pores. You can also apply the moisturizer right after having a bath as the skin is damp at that time and helps lock in the moisture.
Choose Apt Sleepwear
When you are suffering from eczema, your skin tends to become sensitive. Owing to this, when you got to bed, you should avoid wearing clothes made of fabric that is too rough or made from harsh fabric.
Ideally, you should go for loose, airy, and smooth fabrics that easily absorbs moisture. As per a study conducted by Department of Dermatology, University Hospital Case Medical Center, Cleveland, Ohio, USA, it was found that people suffering from eczema should go for Lyocell fabric as it is soft, wrinkle resistant, controls temperature, and controls moisture.
Choose Linens Smartly
The material of the linens also does play a pivotal role as it does affect your body temperature while you are asleep. You can make the following adjustments to your linens and bed –
Ø You should buy protective dust mite covers for your pillows and mattress. For many people suffering from eczema, dust mites have been a common trigger. If this is the case for you, then make sure you have these covers as these will stop you from a frenzy of scratching while sleeping.
Ø If you have blankets, duvets, or quilts, make sure they are made up of materials that can be easily washed and dried. Fabrics that are 100% cotton or bamboo should be your first choice. This means they can be washed quite often to remove dust mites that may affect your sleep.
Develop Good Sleeping Habits
If you are suffering from eczema, you need to develop good sleeping habits. Let us discuss key examples of sleeping habits –
Ø Make sure you avoid eating heavy meals, smoking, and drinking caffeine before sleeping. All these are responsible for disrupting your sleep.
Ø Make sure you make a regular bedtime and wake-up schedule and follow it religiously. This will help train your body to go to sleep and stay asleep.
Ø Make sure you turn off the screens of your computer or mobile phones before you go to sleep. You will enjoy quality sleep in a dark environment. With the help of visual cues such as a dark room, you will have a better night’s sleep.
Ø You should engage yourself in doing recreational things about an hour before you go to bed. You can meditate, take a bath, read your favorite book, listen to light music, etc.
Take a Shower Before You Sleep

If you are looking for the best preventative measure to avoid scratching at night, then make sure you take a bath before you go to bed. After taking a bath, your next move should be to apply your topical medications and moisturizer and then go to bed.
Sleep Aids
If you are still not able to sleep, you can try a sleep aid. Melatonin and Benadryl are two of the most popular ones. The best part is that they are easily available and they can be safely taken together. Have a word with your dermatologist to fix the best dose that fits your needs.
Using Lavender Essential Oil
Since, lavender has antifungal, sedative, calming, and anti-inflammatory properties; it can help to keep eczema at bay. The oil cleanses your skin and reduces irritation and redness.
You can add ten drops of Lavender Essential Oil with one tablespoon of coconut oil (you can use almond oil as well) and rub on the affected areas. The aroma of the oil will help you sleep when you are feeling intense itching.
Wrap Up
If you are suffering from eczema, make sure you work with your physician to make adjustments in your medications to improve your sleep. Besides, you can also discuss various triggers and daily habits that help ease your sufferings.